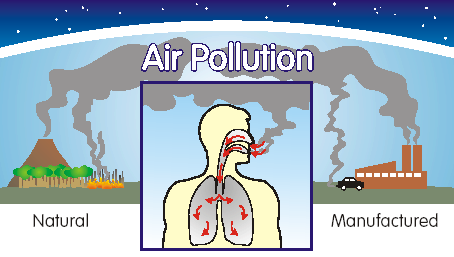
 There are many forms of air pollution. There is no doubt that air pollution is not healthy. The uncertainty is at what level is it an acceptable risk. The one of concern in this study is the finest of particulate matter. The largest study yet to investigate the links between fine air-borne particulate matter (PM) and patient survival after hospital admission for acute coronary syndrome (ACS) found death rates increased with increased exposure to PM2.5 — tiny particles that measure 2.5 micrometers in diameter or less, approximately 30 times smaller than a human hair. The amount of PM in the air is measured as micrograms per cubic meter of air. The main sources of PM2.5 are emissions from road traffic and industry, including power generation.
There are many forms of air pollution. There is no doubt that air pollution is not healthy. The uncertainty is at what level is it an acceptable risk. The one of concern in this study is the finest of particulate matter. The largest study yet to investigate the links between fine air-borne particulate matter (PM) and patient survival after hospital admission for acute coronary syndrome (ACS) found death rates increased with increased exposure to PM2.5 — tiny particles that measure 2.5 micrometers in diameter or less, approximately 30 times smaller than a human hair. The amount of PM in the air is measured as micrograms per cubic meter of air. The main sources of PM2.5 are emissions from road traffic and industry, including power generation.
Air pollution is a significant risk factor for multiple health conditions including respiratory infections, heart disease, and lung cancer, according to the WHO. The health effects caused by air pollution may include difficulty in breathing, wheezing, coughing and aggravation of existing respiratory and cardiac conditions. These effects can result in increased medication use, increased doctor or emergency room visits, more hospital admissions and premature death. The human health effects of poor air quality are far reaching, but principally affect the body’s respiratory system and the cardiovascular system. Individual reactions to air pollutants depend on the type of pollutant a person is exposed to, the degree of exposure, the individual’s health status and genetics.
Dr Cathryn Tonne, lecturer in environmental epidemiology at the London School of Hygiene & Tropical Medicine (London, UK) said: “We found that for every 10µg/m3 increase in PM2.5 there was a 20% increase in the death rate. For example, over one year of follow-up after patients had been admitted to hospital with ACS, there would be 20% more deaths among patients exposed to PM2.5 levels of 20 µg/m3, compared to patients exposed to PM2.5 levels of 10µg/m3.”
Dr Tonne and her colleague Paul Wilkinson, professor of environmental epidemiology at the London School of Hygiene & Tropical Medicine, estimate that death rates would be reduced by 12% among ACS patients if they were exposed to naturally occurring PM2.5 rather than the higher levels they were actually exposed to. This translates to 4,783 deaths occurring earlier than they should do, due to exposure to PM2.5 from man-made sources.
The researchers linked records of 154,204 patients who survived hospital admission for ACS in England and Wales between 2004-2007 with modeled average air pollution concentrations for 2004-2010 for these areas. The patients were followed up until the end of the study in April 2010 or their death, whichever occurred earlier. During the average follow-up time of 3.7 years, there were 39,863 deaths. The researchers adjusted their results to take account of the patients’ sex, age, medical history, treatments and drugs, whether or not they smoked, socioeconomic factors such as income, education and employment, and where they lived.
The air pollution modelling of average exposures for different regions of the country showed the highest average exposures to PM2.5 and other air pollutants in London (an average of 14.1 µg/m3), while the North East of England had the lowest exposure (an average of 8.4 µg/m3). However, people’s individual exposure to PM2.5 varied widely within each region.
Evidence has been growing that exposure to air pollution is associated with the development of heart disease, but, so far, few studies have investigated its effect on survival after heart attacks (myocardial infarction) and the findings have been inconsistent. In addition, it is known that patients from poorer backgrounds often live in more deprived areas with higher levels of air pollution and that they tend to do less well after a diagnosis of heart problems than patients of a higher socioeconomic status.
“Our findings confirm an association between PM2.5 and increased rates of death in survivors of ACS. Our findings also show that PM2.5 exposure contributes only a small amount to differences in survival after ACS among people living in areas with different socioeconomic conditions after accounting for factors such as smoking and diabetes.”
“The implication is that while reducing levels of PM2.5 will lead to increased life-expectancy and is an important public health priority, it isn’t likely to reduce socioeconomic inequalities in prognosis very much. There are likely to be many other factors that are more important than PM2.5 exposure in explaining socioeconomic inequalities in prognosis, and this requires further investigation.”
The study’s strength was in its size and amount of detailed data available about the patients. A limitation was that the researchers lacked specific causes of death and so were unable to discover how many were heart-related, although they suspect the majority were. Exposure to air pollution was based on where the patients lived and did not take account of amounts of time spent traveling or away from home.
Source : ENN